Deciding when to start dialysis can be a daunting experience for patients and their families. The creatinine level in the blood is a crucial factor that plays a significant role in this decision-making process. Creatinine is a waste product produced by muscle metabolism and is typically filtered out of the bloodstream by the kidneys. When kidney function declines, creatinine levels rise, signaling the need for intervention. The timing of initiating dialysis can vary widely depending on individual circumstances, kidney function, and overall health. Understanding the relationship between creatinine levels and the need for dialysis can empower patients and their families to make informed decisions about their treatment options.
In this article, we will explore various aspects of dialysis, including what creatinine levels indicate, when to consider starting dialysis, and how these decisions are made by healthcare professionals. It’s essential to grasp the nuances of kidney function and how it affects overall health, as this knowledge can help alleviate some anxiety surrounding this critical stage of treatment. With a clearer understanding of when to start dialysis based on creatinine levels, patients can take charge of their health and engage in meaningful discussions with their healthcare providers.
Throughout this article, we will answer some common questions regarding dialysis and creatinine levels, providing a comprehensive overview that will serve as a valuable resource for patients facing chronic kidney disease. Let’s delve into the intricate balance between kidney function and the timing of dialysis initiation.
What is Creatinine and Why is it Important?
Creatinine is a chemical waste product that is generated from muscle metabolism. It is produced at a relatively constant rate and is usually filtered out of the bloodstream by the kidneys. The measurement of creatinine levels in the blood provides critical insights into kidney function and overall health. When the kidneys are functioning properly, they effectively remove creatinine from the bloodstream, maintaining normal levels. However, as kidney function declines, creatinine levels can rise, signaling the potential need for dialysis.
When Should You Start Dialysis Based on Creatinine Levels?
Determining the right time to start dialysis is not solely based on creatinine levels but also considers other factors such as symptoms, overall health, and the rate of kidney function decline. Generally, dialysis is considered when creatinine levels reach approximately 6.0 mg/dL or higher, but this threshold can vary. The decision to initiate dialysis is often personalized and should involve discussions between the patient and their healthcare team.
What Other Factors Influence the Decision to Start Dialysis?
In addition to creatinine levels, several other factors can influence the decision to start dialysis, including:
- Symptoms of kidney failure, such as nausea, fatigue, and fluid retention.
- Other lab results, including electrolyte imbalances (e.g., high potassium levels).
- Overall health status and the presence of other medical conditions.
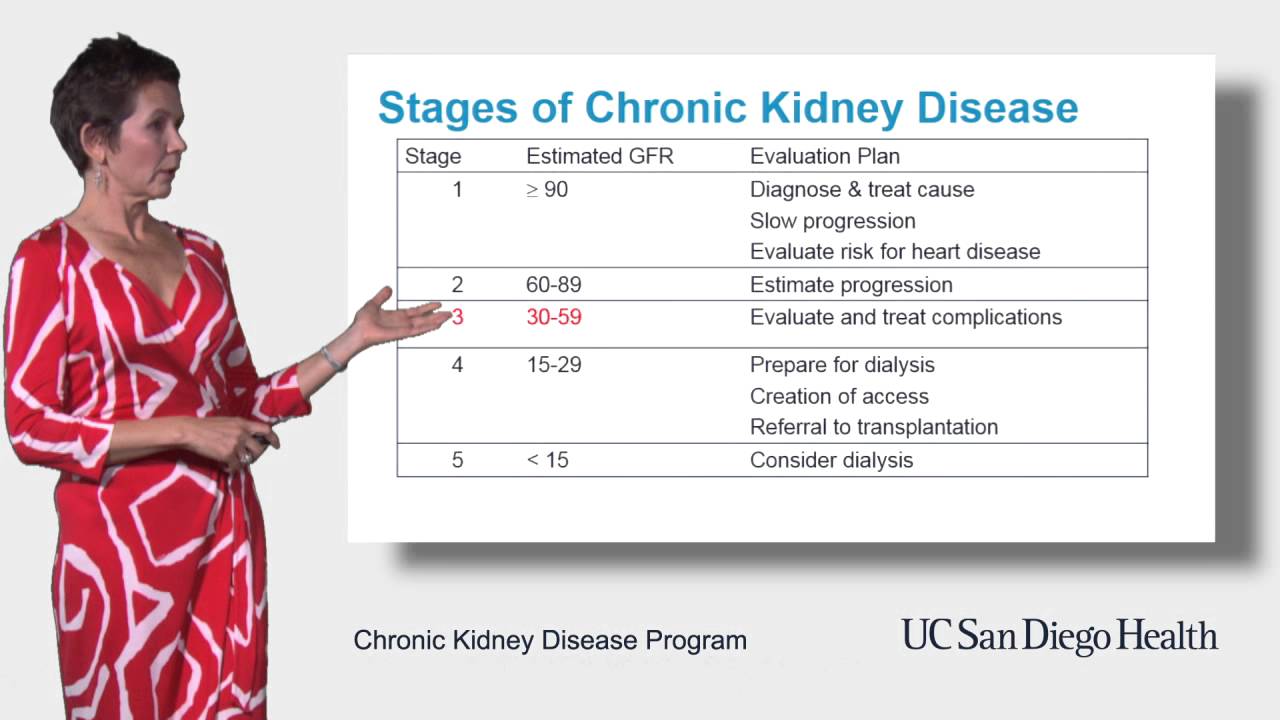
- Rate of kidney function decline as measured by glomerular filtration rate (GFR).
How Can You Monitor Your Creatinine Levels?
Monitoring your creatinine levels is an essential part of managing kidney health. Regular blood tests can help track changes in creatinine levels over time. Patients with chronic kidney disease (CKD) should have their kidney function assessed periodically, allowing healthcare providers to make timely recommendations regarding dialysis initiation. Maintaining open communication with your healthcare team is crucial in understanding your kidney health and when to start dialysis based on creatinine levels.
What Are the Symptoms Indicating the Need for Dialysis?
While rising creatinine levels are a key indicator of declining kidney function, patients may also experience various symptoms that suggest the need for dialysis, such as:
- Severe fatigue and weakness.
- Persistent nausea and vomiting.
- Loss of appetite and weight loss.
- Shortness of breath due to fluid overload.
- Swelling in the legs, ankles, or feet.
These symptoms can significantly impact a patient’s quality of life and may prompt discussions with healthcare providers about when to start dialysis.
How Does Dialysis Work?
Dialysis is a medical procedure that helps remove waste products and excess fluids from the blood when the kidneys are unable to perform this function. There are two main types of dialysis: hemodialysis and peritoneal dialysis. Hemodialysis involves using a machine to filter blood through a dialyzer, while peritoneal dialysis utilizes the lining of the abdominal cavity as a natural filter. Understanding how dialysis works can help patients feel more informed and prepared for the treatment process.
What Are the Risks of Delaying Dialysis?
Delaying the initiation of dialysis can have serious implications for a patient’s health. High levels of creatinine and waste buildup in the blood can lead to complications such as:
- Cardiovascular issues, including heart disease.
- Fluid overload, causing difficulty breathing.
- Electrolyte imbalances, leading to muscle cramps and irregular heart rhythms.
It is crucial to weigh these risks against the readiness for dialysis and to have open discussions with healthcare providers about the best course of action.
Conclusion: When to Start Dialysis Based on Creatinine Levels?
In conclusion, understanding when to start dialysis based on creatinine levels is essential for patients with chronic kidney disease. While creatinine levels are a significant factor in determining the need for dialysis, other clinical signs, symptoms, and individual circumstances must also be considered. Regular monitoring of kidney function and open communication with healthcare providers can empower patients to make informed decisions about their treatment options. Ultimately, the goal is to maintain quality of life while effectively managing kidney health.
Article Recommendations
- Pioneer Dj
- Kill Fleas In House
- How To Make Raphael In Infinite Craft
- Dinosaur Dung
- How Tall Sarah Jessica Parker
- Personal Wifi
- Japanese Watch Brands
- Lola Consuelos Weight Loss Ozempic
- Sheryl Lowe Age
- Bang On Casino